On this 30th anniversary of the International Day of Older Persons, the Australian Government welcomes the COVID-19 report from the Royal Commission into Aged Care Quality and Safety, which has been tabled in the Australian Parliament today.
The Royal Commission’s report tells us the COVID-19 pandemic has been the greatest challenge Australia’s aged care sector has faced and makes six recommendations to better prepare the aged care sector, its staff and residents for any future outbreaks.
The Government accepts all six recommendations in the report and has already made substantial progress on four of them.
The recommendations build on the Government’s existing COVID-19 measures.
The Government will invest $40.6 million in our initial response to the Royal Commission’s report and recommendations.
It has been continuously building and adapting the National Response Plan for COVID-19 in aged care since January 2020, with the aged care sector and with state and territory governments and health authorities, incorporating lessons learned from Australia and other countries.
We have invested more than $1.6 billion to support senior Australians in aged care since the start of the COVID-19 pandemic. The investment includes an additional $734.8 million announced in August to extend support for the sector’s response to the pandemic as part of the aged care response plan.
Wherever there are high rates of community transmission, the risk to older people and particularly those in residential aged care increases as demonstrated in Victoria.
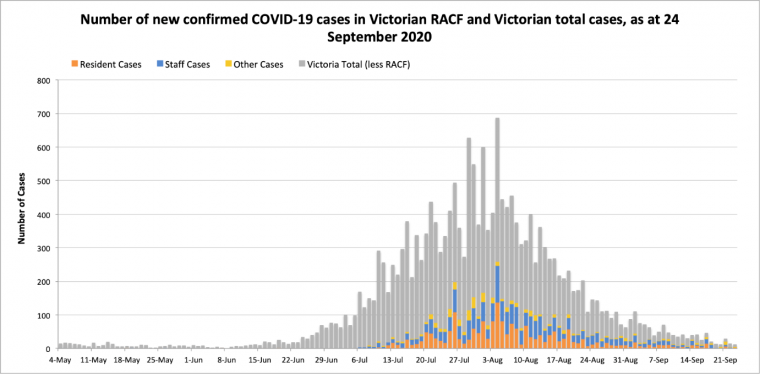 Show description of image
Show description of imageNumber of new confirmed cases COVID-19 RACF and Victorian total cases, as at 24 September 2020.
Recommendations:
Recommendation 1
The Government accepts the recommendation.
It will report to Parliament by no later than 1 December 2020 on the implementation of the Royal Commission’s recommendations.
Recommendation 2
The Government accepts the recommendation.
The Government has announced two packages to provide additional funding for staffing which supports visitations to aged care facilities by families and friends of residents.
In August, the Government committed an additional $245 million to support providers with COVID-19 related costs, including supporting communication with families and managing visitation arrangements, building on the first payment of the COVID supplement of $205 million announced in May.
The Government is also providing $12.5 million to support residents and their families with enhanced advocacy services and increased availability of grief and trauma services associated with a COVID-19 outbreak.
In addition, the Government will bring forward the introduction of the Serious Incident Response Scheme (SIRS) and invest an additional $29.8 million in the SIRS for residential aged care.
Legislation to support SIRS will be introduced to parliament in the spring sitting for the scheme to commence in early 2021.
This builds on earlier investments totalling $26.3 million to establish the system for reporting abuse or serious incidents in aged care facilities.
As part of the SIRS, residential aged care providers will be required to manage all incidents, with a focus on the safety and wellbeing of consumers and reducing preventable incidents from reoccurring.
Reporting under the SIRS will include a broader range of incidents, including neglect, psychological and emotional abuse and inappropriate use of physical or chemical restraint.
Significantly, the SIRS will also lift the current exemption on the reporting of resident-on‑resident incidents, where the perpetrator has an assessed cognitive impairment.
As the Royal Commission Interim Report states: “Informal carers, often family members who supplement the care provided in aged care homes, also play a critical role as the ‘eyes and ears’ – monitoring the quality of care their loved ones receive.”
The SIRS will provide an additional level of assurance when facilities, due to COVID-19, will still need to place a level of restrictions on visitations.
Recommendation 3
The Government accepts the recommendation.
While the Government has introduced a range of measures to support the mental health of residents of aged care facilities, it will continue to implement further measures.
The Government will provide additional funding to support increased access by residents to allied health services during the pandemic and will work with the sector to design and implement these measures.
Recommendation 4
The Government accepts the recommendation.
The Government has a specific national plan for aged care – the CDNA Guidelines for the Management of Outbreaks in Residential Care, which has been updated on two occasions, and which augments the Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID‑19).
The national plan for aged care will continue to be updated incorporating the latest available information and released soon as Stage 7 of the National COVID-19 Aged Care Plan for the consideration by National Cabinet.
The Aged Care Advisory Group, established on 21 August 2020 under the Australian Health Protection Principal Committee (AHPPC), will be made permanent.
The other elements of this recommendation have already been undertaken or are in progress and will also be put to National Cabinet for consideration.
Recommendation 5
The Government accepts the recommendation.
Funding totalling $245 million will be paid to providers from October 2020 to support
COVID-19 efforts.
It will mandate that aged care providers have trained infection control officers as detailed in this recommendation.
In addition, the Government today announces it will invest a further $10.8 million to enhance the skills and leadership qualities of aged care nurses to ensure older Australians receive the best care possible.
This investment will expand the Australian College of Nursing scholarship program, establish an Aged Care Transition to Practice Program, and create a skills development program for nurses and personal care workers in aged care.
Recommendation 6
The Government accepts the recommendation.
The Government has been working with state and territory governments to implement a decision of National Cabinet of 21 August to implement additional face-to-face infection control training and establish joint approaches to the management of outbreaks.
The Government thanks Australia’s frontline aged care workers and Commonwealth, state and territory public health officials. We are deeply aware of the tragic losses that followed the global pandemic and community transmission.
Every life lost to the pandemic is a tragedy.
But the collective efforts of our health workers and health officials and our COVID-19 Aged Care Plan have helped save thousands of lives and placed Australia at the forefront of the global response to COVID-19.
The Government’s actions to protect aged care have been and continue to be based on four key pillars:
Minimise Community Transmission
Controlling community transmission is the best defence we have in protecting vulnerable older Australians in aged care. Under the auspices of the Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID-19) action is being taken by the Commonwealth, states and territories to minimise community transmission including through:
- Minimising the spread of the disease into and across Australia including through quarantine arrangements and effective contact tracing and tracking
- Preparing the health system for increased numbers of patients
- Managing COVID‑19 cases
- Improving understanding of the virus and how it is transmitted
- Provision of information to help manage the risk of exposure and reduce spread
- Vaccination – consideration of the aged care sector in a potential COVID-19 vaccine program
Surge workforce
The Government is providing critical surge workforce support to residential aged care facilities impacted by a COVID-19 outbreak. To date, more than 33,000 shifts have been filled by a Commonwealth-funded surge workforce including GPs, nurses, care workers, allied health workers, executive and ancillary staff.
The Victorian Aged Care Response Centre (VACRC), a joint initiative of the Commonwealth and Victorian Government, was established on 25 July 2020 to co-ordinate and expand resources to tackle the challenge of COVID-19 in residential aged care services.
Under the direction of the VACRC, clinical health staff provided through health services are also assisting to fill critical workforce shortages in residential aged care facilities, with 4,778 shifts filled to date. The VACRC has also assisted the aged care response to COVID-19 through the following activities:
- Australian Defence Force (ADF) personnel have visited 592 aged care facilities.
- 40 personnel from AUSMAT have completed 174 visits to 80 facilities.
- Western Health has provided assistance in prevention measures at 37 aged care facilities.
- 12 National Aged Care Emergency Response (NACER) teams, 76 personnel have been deployed to fill roles across the sector, including nursing, personal care, and cleaning.
- Deployment of TAS, WA, and SA government teams to support operations in residential aged care facilities.
- 101 Residential Aged Care Assistants and Safety Observers have been deployed by the Response Centre to 24 facilities.
- Regular Zoom meetings are being conducted with staff at aged care facilities to assist with return to work arrangements.
Public and private hospitals agreement
These historic agreements between the Commonwealth and each state and territory government alongside the private hospital sector, has ensured the full resources of Australia’s world class health system could be directed to the care of those who needed it. The $1.7 billion private hospital agreement has been instrumental in enabling more than 500 aged care residents to be transferred to private hospitals during the current Victorian second wave.
In addition, it has supported the in-reach of services from hospitals to aged care facilities to provide further clinical care.
Since February 2020, the Government has been working with the states and territories to ensure aged care facilities have sufficient supplies of personal protective equipment. To date, the National Medical Stockpile has provided aged care facilities with approximately:
- 17 million masks
- 4 million gowns
- 11 million gloves
- 4 million goggles and face shields
- 85,000 bottles of hand sanitiser
- 160,000 clinical waste bags.
Universal testing of staff and residents
Immediate testing is provided to staff and residents in a facility to seek to minimise a potential outbreak. Through this in-reach program, more than 152,000 tests at more than 11,000 site visits to 2,000 aged care facilities across Australia have been undertaken. The Government has also provided Medicare funded bulk-billed testing for aged care workers, including those who are asymptomatic. As Victoria starts to recover, this testing will be bolstered to safeguard against a risk of further outbreaks.
Additional investments to support the reform of the aged care sector will be announced as part of the Government’s 2020-21 Budget, to be delivered on 6 October.
Following a request from the Royal Commission, the Government agreed to extend its reporting period for a further three-and-a-half months due to the impact of COVID-19. This enabled the Royal Commission to examine the initial impact of COVID-19 on aged care and the response to date.
We thank the Commissioners for the COVID-19 report and for their work so far, and look forward to receiving their Final Report in February next year.
A summary of the measures to support the aged care sector and key activities undertaken by the Australian Government since the start of the pandemic is attached.
Australian Government funding in response to COVID-19 in aged care – overarching announcements
| Date | Measure | Amount |
|---|---|---|
6 March 2020 – with subsequent additions | Commonwealth contribution to cover 50 per cent of the additional costs incurred by state and territory health services as a result of the diagnosis and treatment of patients with COVID‑19, those suspected of having the virus or activities to prevent the spread of it. This support is uncapped and demand driven. | $3.1 billion |
11 March 2020 – with subsequent additions | Inreach pathology testing in aged care and bulk billed Medicare testing for asymptomatic aged care workers. | $146 million |
11 March 2020 | Workforce preparedness measures – ensuring aged care workers are educated and trained in infection control and enable aged care providers to hire extra nurses and workers for both residential and home care | $101.2 million |
20 March 2020 | Temporary funding to support aged care workforce continuity, including a workforce retention bonus for aged care workers | $444.6 million |
29 March 2020 | Provided to the Community Visitors Scheme and support extra staff to train volunteer visitors to connect with older people in aged care online and by phone | $10 million |
31 March 2020 | Private Hospital Viability Agreement to ensure private hospitals maintain capacity to support the needs of aged care patients, long-stay public hospital National Disability Insurance Scheme participants and general needs patients. | $1.7 billion |
31 March 2020 | Meals On Wheels Programs Reinforced to Help Senior Australians at Home | $59.3 million |
1 May 2020 | COVID-19 Payment (new supplement) for Residential Aged Care | $205 million |
25 May 2020 | Improve palliative care in aged care facilities. The funding will help reduce the physical and emotional distress for individuals who require palliative care and their families | $57 million |
28 May 2020 | Communication package for two new initiatives to prevent loneliness and social isolation for senior Australians | $6 million |
21 August 2020 | Additional support to the Aged Care Sector to increase National Preparedness and respond to the State of Disaster in Victoria | $171.5 million |
31 August 2020 | Extend support for the aged care sector’s response to COVID-19, announced in March and subsequently as part of the Aged Care response plan | $563.3 million |
Key steps taken by the Australian Government to respond to COVID-19 in aged care – planning and preparedness
Stage 1 – Initial Response Plan:
- January – development of an overarching plan for management of COVID-19 for
Australia through the Australian Health Protection Principal Committee (AHPPC)
- 31 January – fact sheets issued on COVID-19, including for aged care
Stage 2 – Release of National Response Plan:
- 18 February – the overarching plan for management of COVID-19, the Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID-19) released
- 27 February – pandemic declared and response plan activated
- 27 February – Letter from CMO to aged care providers which included the Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID-19) and the Communicable Diseases Network Australia (CDNA) National Guidelines for Public Health Units in the Series of National Guidelines (SoNGs)
- 12 March – aged care rapid response team in Department of Health established.
Stage 3 – National Plan and Guidelines for COVID-19 outbreaks in residential aged care:
- 2 March – Aged Care Quality and Safety Commission (ACQSC) Commissioner letter to all aged care service providers regarding planning and preparing for COVID-19
- 6 March – Aged Care Preparedness Forum with Minister Colbeck, Chief Medical Officer (CMO) and Aged Care Sector
- 11 March – $101.2 million in workforce preparedness measures – ensuring aged care workers are educated and trained in infection control and enable aged care providers to hire extra nurses and workers for both residential and home care
- 12 March – AHPPC released a statement on recommended testing and work restrictions for health and aged care workers
- 12 March – ACQSC Commissioner wrote to all aged care services providing an update on actions to protect the safety and wellbeing of aged care consumers during the COVID-19 outbreak
- 13 March – the CDNA published the National Guidelines for the Prevention, Control and Public Health management of COVID-19 outbreaks in residential care facilities
- 13 March – CMO sent a letter to the aged care sector to outline the Government’s current and future support for the central role they play in the national response, including PPE guidance
- 13 March – Minister Colbeck and specialist medical infection control experts convened an In-Home and Community Aged Care COVID-19 Preparedness webinar
- 16 March – online Infection Control Module “How to protect yourself and the people you are caring for from infection with COVID-19” released
- 17 March – ACQSC Commissioner letter to all aged care service providers regarding the updated regulatory response and access to information and guidance
- 17 March – AHPPC released recommendations to residential aged care facilities ensuring they are prepared to manage outbreaks of COVID-19
- 18 March – restrictions on visitors and staff of aged care facilities announced.
Stage 4 – Workforce and PPE Support:
- 20 March 2020 – $444.6 million in temporary funding to support aged care workforce continuity, including a workforce retention bonus for aged care workers
- 23 March – ACQSC Commissioner letter to all aged care service providers about visitor restrictions
- 24 March – guidance issued to aged care sector on process for ordering PPE supplies
- 24 – 27 March – aged care COVID-19 specific online training modules released
- 8 May – a webinar on outbreak preparation and management held to support providers and their staff.
Stage 5 – Revised National Plan and Guidelines for COVID-19 in aged care:
- 28 March – CDNA published updated COVID-19 guidelines for outbreaks in residential care facilities. Updates focused on:
- clinical presentation in older people and
- infection control guidance
- 2 April – Guide to outbreak management and guidance on alerting the Department about confirmed COVID-19 cases in aged care released
- 2 April – Infection Control Expert Group (ICEG – reports to AHPPC) released guidelines for infection prevention and control in residential aged care
- 2 April – Guide to support home care providers with COVID-19 released
- 3 April – ACQSC Commissioner letter to all aged care service providers regarding a suite of posters to help manage COVID-19 in residential facilities
- 4 April – Guide to support CHSP providers with COVID-19 released
- 7 April – AHPPC released a statement on healthcare workers use of PPE when caring for suspected, or confirmed COVID-19 patients
- 12 April – Minister Colbeck announced workforce contingency measures (surge workforce through Aspen and Mable)
- 21 April – National Cabinet met and discussed the lessons learned from recent COVID-19 outbreaks in residential aged care facilities. National Cabinet acknowledged the critical importance of adequate infection prevent and control measures in minimising the spread of COVID-19
- 22 April – AHPPC updated advice to residential aged care facilities about minimising the impact of COVID-19 released
- 22 April – ACQSC’s Chief Clinical Advisor wrote to residential aged care services on screening people entering residential aged care facilities
- 24 April – Minister Colbeck released media statement about the following:
- social restrictions reiterating AHPPC advice
- eSafety courses to keep senior Australians connected during COVID-19
- personal monitoring technology for senior Australians and
- help for senior Australians to access monitoring technology during self-isolation
- 26 April – COVID safe contact tracing app released
- 1 May – $205 million COVID-19 support package (new supplement) for all residential care aged care providers
- 1 May – National Cabinet endorsed preparation of sector led residential care Visitor Access Code
- 12 May – ‘Industry Code for Visiting Residential Aged Care Homes during COVID-19’ released
- 14 May – legislative amendments passed so that senior Australians not penalised or disadvantaged for moving out of an aged care facility during a crisis
- 19 May – CDNA released guidance for health and residential aged care settings on considering monitoring workers for symptoms of COVID-19
- 21 May – ACQSC released storyboards designed to illustrate key behaviours and priority issues during the COVID-19 pandemic
Stage 6 – Revised National Plan and Guidelines for COVID-19 in aged care:
- 10 June – infographic regarding aged care workers visiting your home published
- 19 June – AHPPC statement to provide updated advice on restrictions on entry to residential aged care facilities, including easing of restrictions released. National Cabinet endorsed on 26 June. Updated Industry Code released on 3 July
- 7 July – Minister Colbeck letter to aged care providers reminding them to have an up to date outbreak management plan
- 9 July – ACQSC Commissioner statement regarding Victorian outbreaks
- 10 July – Commonwealth and NSW Protocol to support joint management of COVID-19 outbreaks in residential aged care facilities released
- 13 July – Minister Hunt and Minister Colbeck distributed a joint media release about PPE use in Victorian aged care services and increased supply through the National Stockpile in response to situation in Victoria
- 14 July -CDNA published updated COVID-19 guidelines for outbreaks in residential care facilities. Updates focused on:
- outbreak identification and management guidance
- roles and responsibilities of Government agencies and
- additional members for Outbreak management team
- 16 July – Additional testing teams deployed to test staff and residents in residential aged care services across metropolitan Melbourne and Mitchell Shire
- 16 July – ACQSC Commissioner statement regarding Victorian outbreaks
- 19 July – additional measures announced to support aged care providers in Victoria
- 24 July – case studies of successful outbreak management and additional information released to help manage outbreaks in residential aged care
- 25 July – announcement of establishment of Victorian Aged Care Response Centre to coordinate and expand resources to manage the outbreaks in Victorian aged care services
- 30 July – ICEG advice on use of PPE by health care workers in areas with significant community transmission released
- 31 July – ACQSC Commissioner letter to aged care providers about checks of infection control and correct use of PPE
- 6 August – ACQSC released guideline, ‘Six Steps to Stop the Spread’
- 7 August – Prime Minister announces National Cabinet to work to develop joint Commonwealth – State plans for aged care response including:
- face-to-face infection control training
- plans for implementation of compulsory actions in areas where there are active cases of COVID-19
- establishment of Coordination Centres in each jurisdiction; and
- an audit of State and Territory emergency response capabilities.
- 21 August – National Cabinet endorsed the Commonwealth, State and Territory Plan to Boost Aged Care Preparedness for a Rapid Emergency Response to COVID-19 including a Guide to the Establishment of Aged Care Health Emergency Response Operations Centres.
- Implementation of the plan is being informed by the second survey of residential and aged care facilities (RACF) preparedness recently conducted by the ACQSC and state and territory audits of preparedness.
- Establishment of a time-limited AHPPC Aged Care Advisory Group is endorsed to support the national public health response to COVID-19 in aged care. The Advisory Group brings together a broad range of critical expertise about the aged care sector, infection control and emergency preparedness, and public health response.
- 21 August – Government announces $171 million in additional support to the Aged Care Sector to increase National Preparedness and respond to the State of Disaster in Victoria
- 24 August – the AHPPC Infection Control Expert Group (ICEG) updated guidelines on cleaning and disinfection of protective eyewear in health and residential care facilities published
- 24 August – Minister Colbeck writes to all aged care providers about the release of the Independent Review of Newmarch House, requesting providers’ commitment to take action in response to the findings
- 31 August – Government announces additional $563.3 million to extend support for the aged care sector’s response to COVID-19, announced in March and subsequently as part of the Aged Care response plan
- 7 September – AHHPC endorses advice from its Aged Care Advisory Group that each state and territory should establish emergency response centres
- 18 September – National Cabinet notes progress underway on 21 August commitments:
- Within each jurisdictions’ public health response structure, a dedicated aged care emergency response team is established and key personnel identified at the state and Commonwealth level.
Additional measures to support senior Australians in residential care and in the community
- 29 March – $10 million provided to the Community Visitors Scheme and support extra staff to train volunteer visitors to connect with older people in aged care online and by phone
- 31 March – $59.3 million – Meals On Wheels Programs Reinforced to Help Senior Australians at Home
- 25 May – $57 million to Improve palliative care in aged care facilities. The funding will help reduce the physical and emotional distress for individuals who require palliative care and their families
- 28 May – $6 million for a Communication package for two new initiatives to prevent loneliness and social isolation for senior Australians







