The Australian Institute of Health and Welfare (AIHW) recently released the latest figures on prostate cancer incidence, mortality, and survival in Australia.
The trends over time are different to the trends we see for many other types of cancer, including a decreasing number of diagnoses since 2009, when cases peaked in Australia. In that year, 22,157 cases were diagnosed, compared to 18,110 cases expected to be diagnosed in 2021. With an ageing and increasing population, we might ordinarily expect to see the number of men diagnosed increase, but this has not been the case.
Why?
According to the AIHW:
“Prostate-specific antigen (PSA) testing and associated changes in guidelines can affect the number of new cases of prostate cancer. PSA testing was introduced in 1987 and is thought to have contributed to the peak in incidence in the 1990s. The PSA threshold at which males were referred for a prostate biopsy was lowered in 2002 and might have contributed to the peak incidence during the mid to late 2000s (Smith et al. 2008).”
That is, testing protocols may have contributed to over-diagnosis and over-treatment in the mid to late 2000s, whereas in recent years a revised set of PSA Test Guidelines (2016) has helped to address this concern, in parallel with the availability of new treatment protocols, such as Active Surveillance and Watchful Waiting, which reduce the potential risk of over-treating prostate cancers that pose minimal risk.
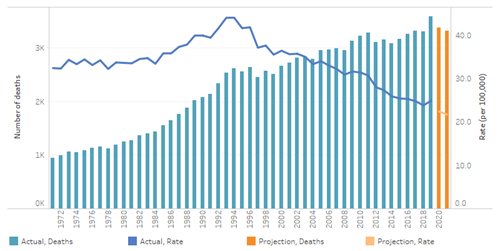
Numbers versus rates
There are two standard measures for understanding big-picture cancer trends, these are the number count of people diagnosed, and the rate, expressed as the number diagnosed per 100,000 people. Due to Australia’s ageing and increasing population, and the link between ageing and cancer risk, it is common to see the number of Australians diagnosed with cancer increase, while overall rates trend downwards, thanks to better prevention strategies for many cancer types, and improved methods of detecting more common cancers in their earliest stages and effectively treating them.
Expressed in charts, this is what the trends look like for prostate cancer incidence and mortality in Australia for the period from 1982 to 2019:
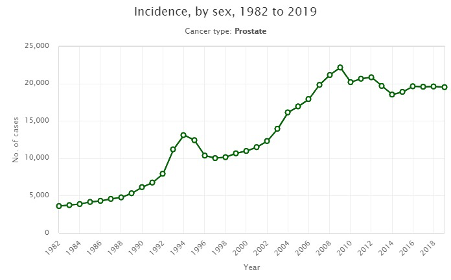
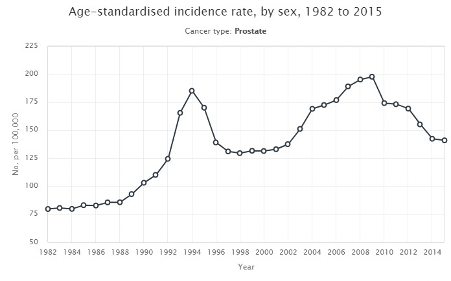
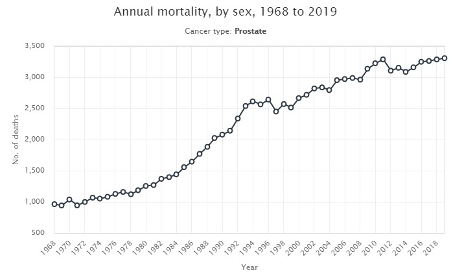
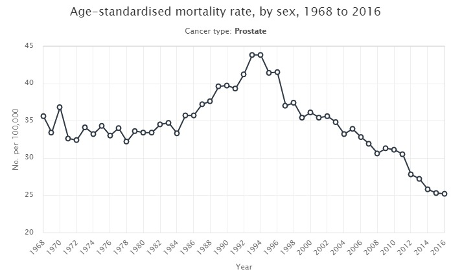
Source: https://ncci.canceraustralia.gov.au/cancer-types/prostate-cancer
The improved mortality rate is a key measure of success and is reflected in increasingly higher rates of survival over time:
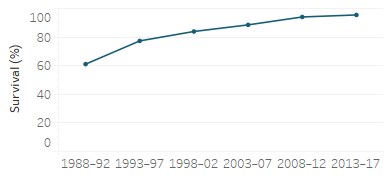
In 1988-1992, on average, 61.1% of males (all ages) diagnosed with prostate cancer survived five years after diagnosis, whereas in 2013-2017, on average, 95.5% of males (all ages) diagnosed with prostate cancer survived five years after diagnosis.
This is tremendous progress, thanks to rapid advances in research and treatment.
According to the government agency, Cancer Australia:
Survival from cancer can be influenced by various factors including demographic characteristics, tumour type, stage of the cancer at diagnosis, other prognostic indicators and availability of treatment. Cancer survival refers to the proportion of patients expected to survive their cancer at a specified point subsequent to the diagnosis of cancer, or from some designated point after diagnosis (conditional survival). It is commonly presented as the probability of surviving their cancer at a specified time after diagnosis, e.g. 5-year or 10-year survival.
The measure ‘5-year relative survival at diagnosis’ is defined as the ratio of the proportion of people who are alive for 5 years after their diagnosis of cancer (observed survival), to the proportion of people in the general population alive over the same time interval (expected survival). Those in the general population are normally matched for age, sex and calendar year to those with cancer. Observed survival is calculated for Australia, using data from population-based cancer registries. Expected survival is calculated from life tables for the entire Australian population.
Survival rates for prostate cancer therefore vary depending on the stage of cancer at diagnosis, the patient’s age, and the characteristics of the cancer itself, among other things.
Incidence
Prostate cancer is the most commonly diagnosed cancer in Australian men. Estimates suggest that 18,110 Australian men will be diagnosed in 2021. (https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/summary).
Estimated most common cancers diagnosed among males, 2020:
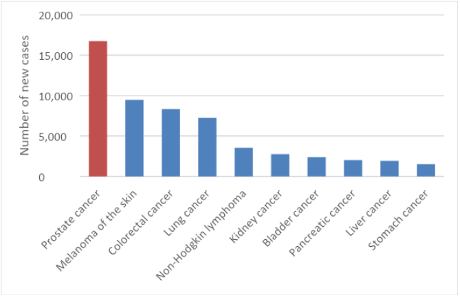
The rate of age-standardised incidence in 2016 was 141 cases per 100,000 males. This is expected to decrease to 110 cases per 100,000 males in 2020.
Evidence shows that incidence rates for prostate cancer increase with age, and are highest among the age group 70-74, decreasing thereafter.
That is, a male’s chance of being diagnosed with prostate cancer increases with his age.
Of the 18,110 Australian males expected to be diagnosed with prostate cancer this year, 407 (2.24%) will be under 49 years of age, 2,888 (15.94%) will be 50-59 years of age and 6,713 (37.06%) will be 60-69 years of age, 5,979 will be aged 70-79 (33.01%), and 2,123 will be over the age of 80 (11.72%).
Mortality
Prostate cancer is the second most common cause of cancer-related deaths in Australian males after lung cancer. Of concern, estimates suggest that 3,323 men will die from prostate cancer in 2021. The charts below are from the government agency Cancer Australia.
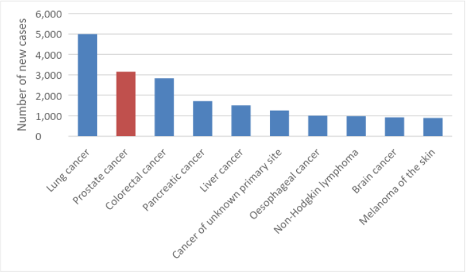
The rate of age-standardised mortality in 2018 was 23.8 deaths per 100,000 males. This is expected to decrease slightly to 21.7 deaths per 100,000 males in 2021.
How does cancer stage influence survival?
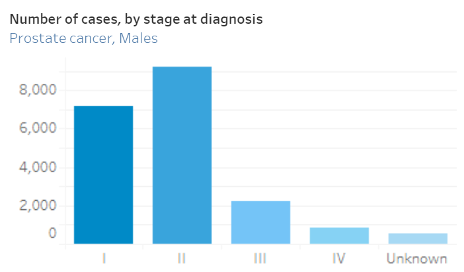
Cancer stage refers to the extent of spread of cancer – the higher the number between I and IV, the further the cancer has spread. In Australia, five-year relative survival for prostate cancer diagnosed at Stage I is 100%. The survival rate for Stage 4 cancers is just 36.4%.
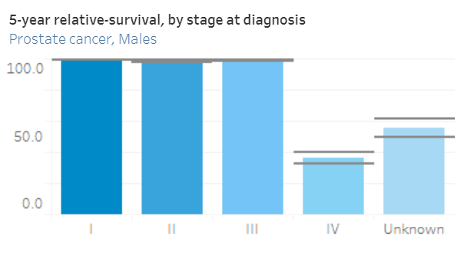
These rates highlight the importance of detecting prostate cancer at its earliest stages in order to improve survival outcomes. Yet only 36% of prostate cancers are detected at Stage I in Australia, 46% are detected at Stage II, 11% are detected at Stage III, 4% are detected at Stage IV, and in about 3% of cases the stage at diagnosis is unknown.
Demographic disparities
Those in marginalised groups commonly experience poorer outcomes when it comes to cancer survival. This is true for prostate cancer, and in some instances the gap has widened over recent years, meaning that advances in research and treatment have not been shared equitably across the population. For Australian males affected by prostate cancer, evidence suggests those in regional and rural areas, and those who live in areas of relative socio-economic disadvantage, experience higher rates of mortality and lower rates of survival.
The mortality rate for Australian males who reside in regional and rural areas is 24% higher – at a rate of 56.9 per 100,000 compared to 45.8 per 100,000 for those in urban areas (2007). Likewise, regional and rural males had a five-year relative survival rate of 88% compared to a survival rate of 91% for males from urban areas over the same time period (2000-2004). You’ll find that data here: https://www.mja.com.au/journal/2011/194/6/urban-rural-differences-prostate-cancer-outcomes-australia-what-has-changed.
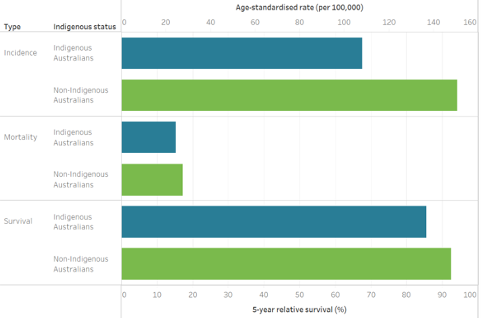
Among Indigenous Australians, incidence and mortality rates are lower than rates for non-Indigenous Australians, due to a range of factors associated with overall health status and life expectancy, but in spite of this, Aboriginal and Torres Strait Islander men who are diagnosed with prostate cancer still experience comparatively poor survival outcomes. For the period from 2007 to 2014, these men had an 86% chance, on average, of living for five years after their diagnosis, compared to a 92% survival rate for non-Indigenous Australians.
Family history
Awareness of your family history of prostate cancer is key to early diagnosis and survival of the disease:
- If your father or brother have ever been diagnosed with prostate cancer, you have twice the average risk of developing the disease.
- If you have two or more close male relatives who have been diagnosed, your lifetime risk of developing prostate cancer increases five-fold.
- Your risk also increases if you have a strong family history of breast or ovarian cancer, especially if a BRCA1 or 2 gene mutation was involved.







