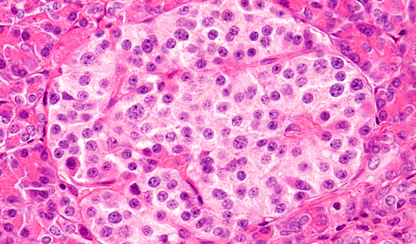
A proof-of-concept study demonstrates that ductal cells derived from the human pancreas can be influenced by pharmacological stimulation to regenerate beta-like cells that functionally release insulin, providing new hope for people living with diabetes.
The preclinical study, conducted by Safiya Naina Marikar from the Baker Heart and Diabetes Institute and published this week in the journal Clinical Epigenetics, demonstrates how drugs can influence pancreatic progenitor cells to reactivate into beta-like producing insulin cells by inhibiting the EZH2 enzyme.
With type 1 diabetes, beta cell damage and destruction mean the pancreas produces little or no insulin. This results in glucose build up in the bloodstream instead of going into the cells. This build-up of glucose in the blood is called hyperglycemia, with the body unable to use the glucose for energy.
Researchers have dedicated enormous time and energy looking at alternatives such as cell replacement therapy and pancreas transplantation — a potential option limited because of the stark reality of donor organ shortage. This approach examines the regenerative capacity of pancreatic cells by stimulating ductal stem cells with small molecule inhibitors as an alternative strategy to restore insulin production for people living with diabetes.
The drugs used in the study include a synthetically designed drug primarily used as a cancer therapeutic (with overexpression of EZH2 found in cancers) and a naturally derived drug that has been tested as a treatment for inflammatory conditions.
PhD student at Monash University, Safiya Naina Marikar, who is based at the Baker Institute in Professor Sam El-Osta’s Human Epigenetics program, says this study suggests that the reprogrammed cells are capable of producing insulin and critical functionality such as insulin secretion in response to glucose stimulation.
Professor El-Osta says this exciting epigenetics work led by early career scientists could have important implications in improving the lives of people with diabetes in coming years.
While more studies are needed to address mechanism and the identity of cell targets to improve methods to reduce the burden of insulin-dependent diabetes, these findings provide an exciting new avenue for the regeneration of beta-cells as a possible alternative source to islet transplantation for people living with diabetes and close that therapeutic gap.
About type 1 diabetes
134,000 Australians are currently living with type 1 diabetes, and it represents 10 per cent of all cases of diabetes and is increasing each year(source). Type 1 diabetes occurs when the cells of the pancreas are destroyed by the body’s immune system, meaning that the body is unable to produce any insulin. It requires treatment with ongoing insulin therapy. It is not caused by lifestyle factors and has no known cause or cure and although it is often diagnosed in childhood, it can occur at any age.








