CERA’s Head of Visual Neovascular Research Dr Luis Alarcon-Martinez is bringing international collaborators together to investigate blood flow in the retina, thanks to a five-year grant from Foundation Fighting Blindness Canada.
Together they’re aiming to gain a deeper understanding of how the retina, optic nerve and brain are impacted in glaucoma.
The most common known cause of glaucoma is too much pressure inside the eye causing damage to the optic nerve.
However, there are also many people who do not experience high eye pressure that still develop the condition.
Dr Alarcon-Martinez says it’s vital to decrease eye pressure, but “we know we are missing something very important about the disease.”
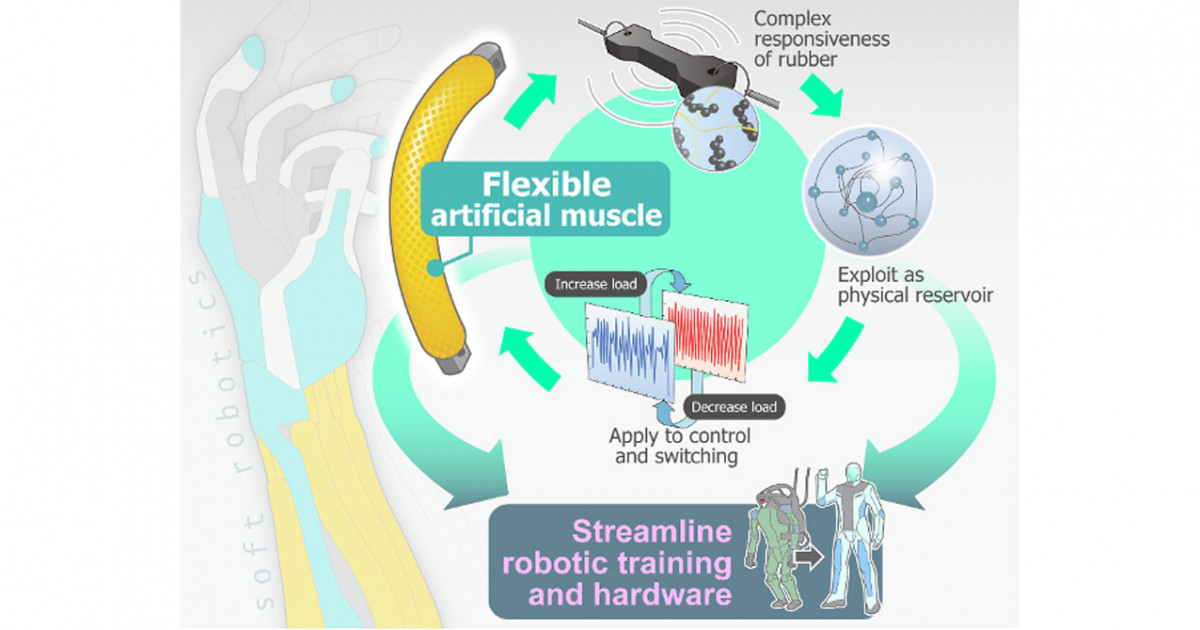
He believes that mechanisms controlling blood flow through our light-sensing nerve cells may hold the key to unlocking this mystery.
“Nerve cells are always getting or using some levels of energy, which is why blood flow is so important to the retina, the optic nerve and the brain,” says Dr Alarcon‑Martinez.
“If you stop blood flow, the nerve cells will die.”
Dr Alarcon‑Martinez is working with Professor Adriana Di Polo from the University of Montreal, who is a global leader in understanding the mechanisms behind glaucoma.
CERA Managing Director Professor Keith Martin will also contribute to the study, and Professor Bang Bui from the University of Melbourne is bringing his invaluable knowledge of living glaucoma models.
“We hope this study lays the groundwork for new treatments aiming to improve blood flow – supplementing current treatments that lower eye pressure,” says Dr Alarcon‑Martinez.
Communication is key
The team will look deep behind the eye using Dr Alarcon-Martinez’s pioneering two-photon microscopy setup – an advanced imaging technique allowing researchers to see living tissue at a scale not possible with other microscopes.
Dr Alarcon‑Martinez and Professor Di Polo previously used two-photon microscopy to discover formerly unseen structures that communicate to regulate blood flow between cells in the retina, optic nerve and brain.
“We are now seeing the importance of this process to diseases, including glaucoma,” says Dr Alarcon‑Martinez.
The light-sensing retina at the back of the eye is made up of many nerve cells, which are constantly using energy to send signals through the optic nerve to our brain.
“Most cells in our body can store energy for whenever needed, but nerve cells don’t have this ability,” says Dr Alarcon‑Martinez.
Instead, they constantly ‘ask’ blood vessels for oxygen and nutrients, which every cell needs to produce energy.
Pericytes are a type of cell that wraps around the blood vessels and controls the amount of blood passing through them.
By looking at a living organism, Dr Alarcon‑Martinez and his team discovered pericytes project very thin tubes called nanotubes.
“Nanotubes send signals between blood vessels to lead blood flow to where energy is needed most,” says Dr Alarcon‑Martinez Dr Alarcon‑Martinez says this communication is disrupted if nanotubes are broken.
Huge potential
The team will use a pre-clinical model of glaucoma developed by Professor Bui to investigate how this communication is affected by the disease – comparing the results with healthy living organisms.
“We’ll be looking at single axons and blood vessels with the aim of detecting how well single nerve cells are working – hoping to see if we can prevent, predict or even give a score of the state of the glaucoma,” says Dr Alarcon‑Martinez.
The team’s findings will also give valuable insights to other CERA research looking at new ways of treating glaucoma, such as Professor Martin’s work into developing a gene therapy to prevent optic nerve damage.
For World Glaucoma Week (10-16 March), we’re shining a light on stories of research and community support that are collectively working towards a common goal: finding new ways of detecting and treating the world’s leading cause of preventable blindness.
Our team investigates how blood is distributed in the retina to help prevent or treat retinal neurodegenerative diseases.