Researchers at Weill Cornell Medicine have found that controlling high blood pressure may not be enough to prevent associated cognitive declines. The findings point to an immune protein called cytokine IL-17 as a culprit for inducing dementia and suggest new approaches to prevent damage to brain cells.
The study, published on Dec. 4 in Nature Neuroscience, uncovered a new mechanism involving increased levels of IL-17 in the brain, which suppressed blood flow to the brain and induced cognitive impairment in a preclinical model of salt-sensitive high blood pressure.
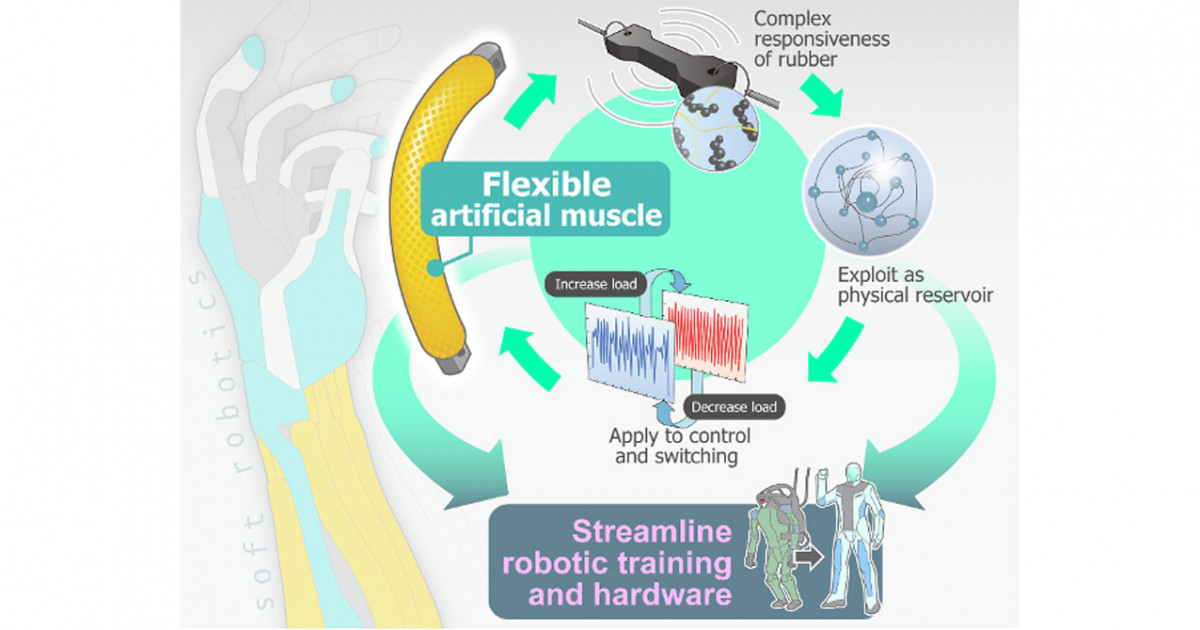
Immune cells producing IL-17 (green) within a sample of the dura membrane that surrounds the brain. IL-17 may promote dementia in those with high blood pressure. Endothelial cells that line blood vessels are tagged magenta.
“An increase in blood pressure is not what hits the brain to cause dementia,” said senior author Dr. Costantino Iadecola, the Anne Parrish Titzell Professor of Neurology and director and chair of the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine. “That may be important for the heart, putting an excessive load that makes the heart pump harder. But as far as cognitive impairment, our data suggest that one of the major causes is this IL-17 immune response.”
High blood pressure affects more than one billion people globally, and approximately half of them have salt sensitivity, an increase in blood pressure associated with higher salt consumption. Making matters more complicated, hypertension is a leading risk factor in dementia, but that relationship is not well understood.
“There has been some debate as to whether managing blood pressure with hypertensive drugs is enough to prevent cognitive decline,” said first author Monica Santisteban, who is currently an assistant professor of medicine at Vanderbilt University Medical Center.
The researchers turned to another piece of the puzzle to better understand the relationship. Hypertension in humans is linked to T cells of the immune system releasing more IL-17, causing increased levels circulating throughout the body. This led them to focus on IL-17 and its potential connection to cognitive health. Normally, IL-17 is part of the immune response to pathogens but can contribute inflammatory diseases.
The researchers replicated cognitive issues in a preclinical model with increased IL-17 levels. IL-17, produced by T cells in the gut and the circulatory system, is involved in decreasing blood flow to the brain by acting on endothelial cells that line the inside of blood vessels. Lack of necessary blood flow can damage brain cells. So, the researchers eliminated IL-17 receptors on endothelial cells to block that interaction and to see if this prevented cognitive impairment. However, Iadecola and his team found even after blocking the effects of IL-17 on the brain, cognitive issues remained.
They then examined the protective membrane around the brain called the meninges, since past studies pointed to immune cells, and a potential source of IL-17, in this area. Isolating the dura, the outermost layer of the meninges, the team located T cells that produced IL-17 independent of the gut. They also discovered that the IL-17 was able to infiltrate the brain since the arachnoid, the middle layer in the meninges, was damaged. There, IL-17 interacted with receptors on brain-associated macrophages, another type of immune cell. This induced oxidative stress that caused tissue injury and suppressed necessary blood flow to the brain.
Surprisingly, when the team eliminated the T cells in the meninges, or the macrophages in the brain, they restored full cognitive function. These findings uncover a previously unknown critical role that T cells in the meninges and IL-17 play in the cognitive impairment associated with salt-sensitive hypertension.
Iadecola and Santisteban believe this finding creates opportunities to study new combination therapies. Avenues could include adding IL-17 inhibitors to treat cognitive impairment with conventional treatments for reducing blood pressure. Currently, IL-17 inhibitors are commonly used to treat autoimmune diseases, such as psoriasis, a skin condition.
“More research will be looking at what other cell types in the dura are contributing to the relationship between hypertension and dementia,” Santisteban said. “But the biggest takeaway here is that managing blood pressure may not to be enough to manage cognitive decline.”
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see the profile for Dr. Costantino Iadecola.
This work was supported by grants from the National Institutes of Health as well as the Leon Levy Fellowship in Neuroscience (MMS). The support from the Feil Family Foundation is gratefully acknowledged.
Lauren Barack is a freelance writer for Weill Cornell Medicine.