Australia’s first dedicated testing facility for protective gowns has been established at Flinders, where research is also starting on improving face mask safety.
The two Flinders University R&D projects, supported by Flinders Foundation grants, aim to make more locally-made personal protective equipment (PPE) available to keep healthcare workers safe from COVID-19 and other infections.
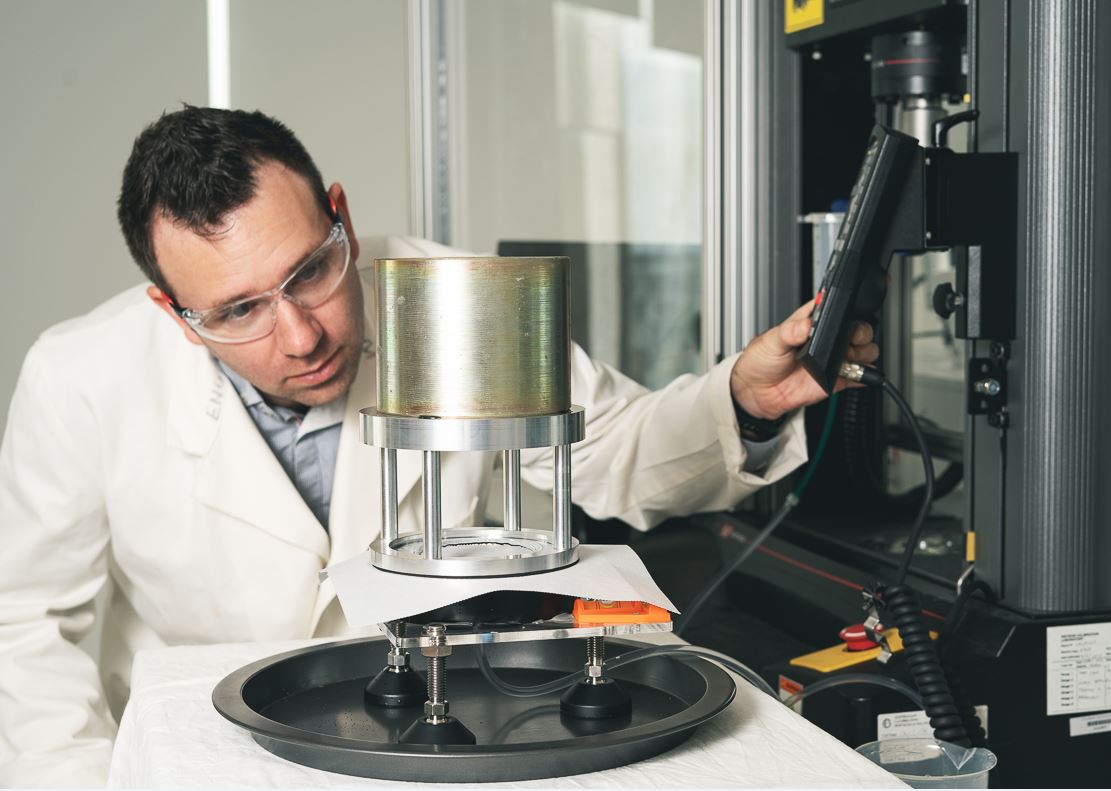
The Medical Device Research Institute (MDRI) researchers at Flinders at Tonsley are testing fabric samples from gown manufacturers for resistance to bacteria, virus and fluids.
And an innovative trial at Flinders Medical Centre will test 3D printed face mask seals moulded to the faces of individual healthcare workers in a bid to reduce the potential for any infection caused by ill-fitting masks when treating COVID-19 and during other high-risk procedures.
MDRI director Professor Karen Reynolds says serious disruption of PPE supplies during the COVID-19 pandemic showed it was now more important than ever to establish an Australian-based gown testing facility. “PPE is necessary for healthcare workers to protect themselves from being infected,” she says. “This includes gloves, medical masks, respirators, goggles, face shields, gowns and aprons.
“During the pandemic, there has been grave concerns for PPE availability as demand for this equipment increased rapidly, and there has also been misuse, hoarding and theft, combined with reduced supply because of transport and export restrictions.
“I don’t think gowns and masks crossed anyone’s mind before now, they were just gowns and masks – but now everyone is talking about PPE and the ramifications of not having a stable supply.”
At present, gowns need to be sent overseas to undergo strict manufacturing and testing standards. But the new Tonsley-based gown testing facility aims to fast-track the process for Australian-based manufacturers and get good quality, safe PPE into hospitals faster.
The $38,000 grant from Flinders Foundation will provide equipment and initial staffing to establish the facility, where various gown fabrics will be tested for their resistance to blood-borne pathogens, as well as undergoing impact penetration and hydrostatic pressure tests for fluids.
Pathogens will also be grown on-site to create an environment where gowns are tested against some of the very viruses and bacteria that cause disease.
“The idea is that manufacturers can bring their gowns here, we can run the tests and they can move forward with production, meanwhile hospital services can be confident their staff are properly protected,” Professor Reynolds says.
Once operational, any tests performed will be done under contract with manufacturers for an appropriate fee.
The gown testing facility builds on a recent move by the State Government, Flinders University and UniSA to develop the South Australian Mask Testing Facility at Tonsley to test respirator and surgical masks produced by local manufacturer Detmold.
“Since the announcement of the mask testing facility, we’ve been inundated by requests to undertake testing for more than 30 companies and healthcare providers from across Australia and New Zealand and we now expect there to be interest in gown testing also,” Professor Reynolds says.

Meanwhile, Flinders University cardiologist, Associate Professor Anand Ganesan, and fellow researcher Darius Chapman will use a mobile phone app to scan the 3D geometry and coordinates of an individual’s face to make a seal which when printed out can comfortably sit between a standard N95 grade face mask and the healthcare worker’s face.
The aim of the new, reusable, custom-made seal is to prevent gaps between the cheek and the nose where viruses, bacteria and fluids can leak through.
“We’ve also seen images of our colleagues, particularly in other parts of the world, with bruises and pressure sores on their nose and cheeks from the force of continually wearing masks with the straps pulled tightly to try to protect themselves,” says Associate Professor Ganesan.
“The human face is so variable and there’s different shapes and sizes for everyone so a generic one size fits all mask won’t capture everyone, so we’ve set about trying to limit the leak from these masks.”
If the trial is successful, the face seals have potential in other industries, such as emergency service fire fighters or even sleep apnoea patients to improve the comfort and efficiency of CPAP machines.







