Are sleeping pills the only solution for insomnia? Not according to Flinders University’s Dr Alexander Sweetman, who says that using self-guided digital behavioural therapy is an alternative solution that should be considered.

Despite a wealth of evidence supporting the effectiveness of cognitive behavioural therapy for insomnia (CBTi), access to this ‘first line’ treatment is extremely limited due to a shortage of CBTi trained psychologists.
In Australia, approximately 90 per cent of primary care patients with insomnia are managed with sleeping pills while only 1 per cent are referred to psychologists for CBTi.
To increase accessibility to CBTi and reduce the reliance on sleeping pills, sleep experts at Flinders University and the University of Western Australia designed and tested the effectiveness of a self-guided digital CBTi program called ‘Bedtime Window’ to treat insomnia.
“We tested a new CBTi program in people with insomnia symptoms throughout Australia and found it very easy to use, delivering significant and sustained improvements in sleep, daytime function and mental health,” says Dr Alexander Sweetman, who led the latest research published in Frontiers in Sleep.
“We know that CBTi improves insomnia, mental health and quality of life and we want to see more people accessing this treatment because it can reduce the need for sleeping pills or other interventions which may not tackle long-term sleep problems,” he says.
Insomnia and obstructive sleep apnoea (OSA) are the two most prevalent sleep disorders and frequently co-occur. Approximately 30-40 per cent of people with insomnia have co-morbid OSA however most people with OSA remain undiagnosed and untreated.
“People with co-morbid insomnia and sleep apnoea (COMISA) generally have worse sleep, daytime function, mental health, physical health, productivity and quality of life when compared to people with neither sleep disorder, and often when compared to people with either insomnia-alone or OSA-alone,” says Dr Sweetman.
“Recent studies found that people with COMISA experience a 50-70 per cent increased risk of mortality over 10-20 years of follow-up, compared to people with neither condition.
“Given the high prevalence and adverse health risks of COMISA, it is vital that we develop and implement an effective evidence-based management approach for this condition,” he says.
“To increase CBTi access for people with COMISA, we developed the self-guided interactive digital CBTi program that is appropriate for people with insomnia-alone and COMISA and compared its effectiveness between people with insomnia-alone, versus comorbid insomnia and high-risk sleep apnoea.”
62 adults with insomnia symptoms used ‘Bedroom Window’ over an 18-month period and reported significant and sustained improvements in symptoms of insomnia and associated mental health symptoms.
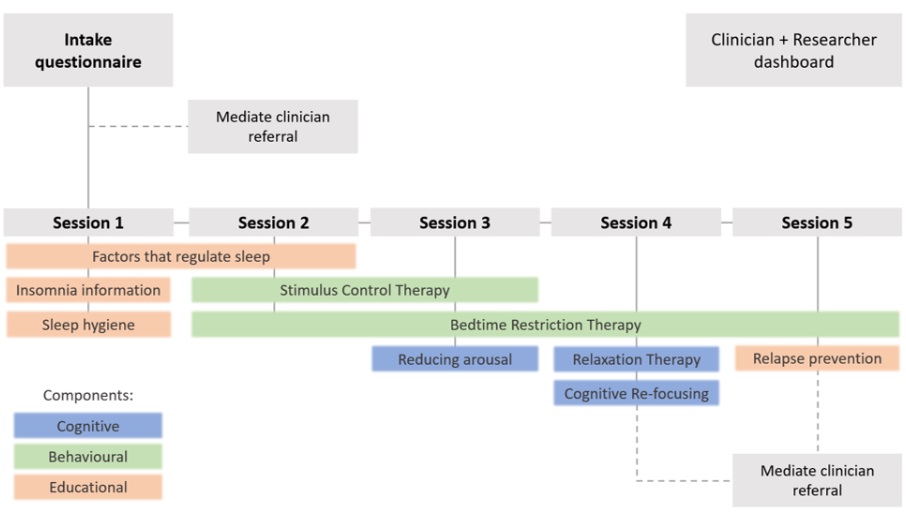
“The program is designed for people with insomnia-alone and COMISA. Each weekly session lasts for approximately 20-30 minutes and includes short videos, images and text-based information,” he says.
“Treatment components include psychoeducation, stimulus control therapy, sleep restriction therapy, relaxation therapy, cognitive therapy and sleep hygiene information.
“The program includes algorithms that continuously assess for symptoms of sleepiness and alertness and provides tailored and interactive recommendations to treat insomnia without worsening levels of daytime sleepiness.
“The positive results of our study highlight the potential to investigate the effectiveness, safety and acceptability of this digital CBTi program in people with a confirmed diagnosis of OSA, before increasing access to people with COMISA throughout the health system,” adds Dr Sweetman.
The article ‘Effect of high-risk sleep apnoea on treatment-response to a tailored digital cognitive behavioural therapy for insomnia: A quasi-experimental trial‘ was published in Frontiers in Sleep by Alexander Sweetman, Chelsea Reynolds, Leon Lack, Andrew Vakulin, Ching Li Chai-Coetzer, Douglas M Wallace, Megan Crawford and Cele Richardson.